Lolita Wsterlund is one of the first women in the world to have a uterine transplant. Now this pioneering surgery is coming to Britain. By Tim Lewis

Moments after giving birth, her son not yet in her arms, Lolita Wsterlund had an urgent fear. Does he have a really big nose? she near screamed. Her partner Patrik, and the doctors and nurses who had performed the caesarean, looked bemused. Almost a year on, Lolita or Lollo to her friends shakes her head at the memory. Its a funny question, but in one picture during the ultrasound it looked like he had a really, really big nose. But they said: No, his nose is just perfect. What a question!
Few pregnancies are entirely straightforward, but Lollos was an especially discombobulating one. It was not the birth so much, though she did experience the dreaded pre-eclampsia and her son arrived hurriedly a few weeks premature. Much more significant was that Lollo herself was born with Mayer-Rokitansky-Kster-Hauser syndrome, a condition that affects around one in 5,000 girls. MRKH sufferers have ovaries, but no uterus. Lollo also had a shortened vagina and only one kidney. She found out when she was 14, in the early 1990s, when she went to the doctors with a pain in her ovaries. After exploratory surgery, she was told she would never be able to get pregnant or carry a baby of her own.
Recalling the birth of her son, Cash-Douglas, Lollo says: Just the whole experience was too big. I guess its big for everyone, but it was too big to go from, Im never going to be able to have a kid To actually having a kid inside me. My own baby.
Lollo, 36, is the beneficiary of the pioneering technique of uterus transplant surgery. Developed in her homeland Sweden, a trial was started with 10 women. The first gave birth in September 2014 and there have since been another four healthy babies born. One of those women is now pregnant for a second time. The uteruses come from live donors in Lollos case, both her sister and her mother offered theirs and the doctors from the University of Gothenburg selected her sisters as she was younger. She is four years older than Lollo and already has four children.

My sister always told me she was going to give me her uterus, says Lollo. She said it the first time when I was 14. Its funny because as teenagers we were always fighting, but when my eldest nephew was born, something happened. I had two choices: either to turn my back on him, because it hurt so bad; or embrace him. And thats when my sister and I got close, like real close. I chose to embrace him, but it was a tough decision and she had a hard time telling me she was pregnant.
As far back as she can remember Lollo had wanted children of her own and, until recently, she was a kindergarten teacher. After her diagnosis with MRKH, she recalls feeling profoundly miserable. She sought out psychologists, but they couldnt help with her grief. She shut her family out. Dating was problematic because there never seemed a good moment to say to a guy that she couldnt have children. Should I tell them at the beginning? she says. Or should I tell them later? But then it would feel like Im cheating or lying. She met her current partner Patrik a decade ago and warmed to him immediately when he told her that he never wanted to get married or have kids. So that sorted it out, Lollo giggles.
Patrik was in for a shock. Lollo first heard about uterus transplants in 1999, after her mother read a story in the papers about a Swedish doctor, Professor Mats Brnnstrm, who was starting experiments on animals. Lollo called him and they had a brief conversation. Years later, she spotted another article which reported that Brnnstrm had received ethical permission to begin trials on humans. Lollo and Patrik, who was warming to the idea of parenthood, had already discussed and rejected adoption. Lollo and her sister toyed with the idea of surrogacy, but it is illegal in Sweden. The trial seemed to be her last hope.
Uterus transplants have a well-earned reputation as a highly complex procedure. The operation was first attempted in Saudi Arabia in 2000, but the implanted organ had to be removed after three months. A woman in Turkey successfully became pregnant in 2011, but miscarried soon after. Using live donors as the Swedish team was attempting to do requires surgeons to remove a small section of the donors vagina without disturbing the vital organs clustered around it. The surgery on Lollos sister, for example, took around 12 hours.
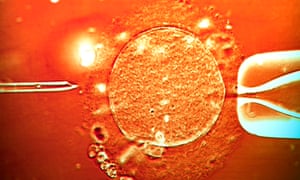
It wasnt straightforward for Lollo, either. She, her sister and Patrik all had to pass rigorous physical and psychological assessments before they were accepted on the Gothenburg trial. The doctors then collected 10 eggs, which they fertilised with Patriks sperm and then froze. The embryos were implanted one at a time. I was getting so scared because he was the sixth try, Lollo recalls. He was number six embryo. So each time the test was negative, I was sad all over again.
Uterus transplants are set to become a reality in Britain soon, too. Last September, a team led by Richard Smith, a gynaecologist and cancer specialist based at Queen Charlottes and Chelsea Hospital in London, was given approval by a research ethics committee to do 10 transplants. The donors will not be live; instead the uteruses will be taken from heart-beating brain-dead cadavers, removed as part of the standard organ-retrieval process. The 10 patients for the trial have not been finalised, but Smith has been meeting potential candidates for years and the numbers have been whittled down from over 500 to 104 to 46. He hopes it will begin on 1 September.
Smith believes there might be 10,000 women in the UK aged between 20 and 40 either without a uterus or with a malformed one. So, what if someone reading this article would like to put themselves forward? Im not saying its impossible, but it is slightly late in the day, says Smith over the phone, as he waits to board a flight to Cork to deliver a lecture on fertility-sparing surgery. But do remember that were trying to set up a programme, which will do 10 experimental cases and hopefully well have many babies. Then in 2020 we hope we will have a sustainable national programme, which will go forwards for keeps.
The British teams criteria, based on the Swedish model, is that a woman should be between 24 and 38 and be incapable of reproduction because of a problem with her uterus. Each applicant is evaluated physically and mentally. Psychologists look at everything from a persons tendency to depression to the stability of their relationship.
Every one of these stories, to be truthful, is a personal tragedy, says Smith. From the girl who discovers when shes halfway through her teens that shes not got a uterus, to the woman who loses her uterus in labour and her baby at the same time. From the woman who loses her uterus because of cancer, to the woman who loses her uterus because of haemorrhage. Their ability to carry a baby has been taken away from them for one reason or another. It is very, very emotive.
Once the 10 have been selected, they will go through IVF to produce a minimum of 10 embryos and they will then unlike Sweden be put on a rota for two years waiting for organs to become available. Here Smith is looking for a female cadaver aged between 18 and 50 who, scans show, has a normal uterus and who has had a baby so that they know the transplanted uterus is functional. He expects around 10 suitable organs a year to become available in the London area and is aiming to do five cases annually.

As a non-vital organ transplant, we are at the back of the queue and thats right and proper, says Smith. The cardiothoracic people retrieve the heart and lungs, then the abdominal surgeons retrieve the liver, kidneys and sometimes the small bowel and pancreas. Then its ourselves.
The Swedish team used live donors because, having a smaller population, they could not rely on a ready supply of cadavers. It is, however, ethically and medically more straightforward to use a recently deceased source. Whether these transplants will be as effective remains to be seen. So far the only successful births have come from women who have received their uterus from a live donor.
In February, the Cleveland Clinic attempted the first uterus transplant surgery in the United States. The womb came from a deceased donor and was implanted into a 26-year-old woman from Texas. Within two weeks, though, the uterus had to be removed because of an infection.
Professor Brnnstrm notes that infections are a risk whether you use live or deceased donors his team has also had failed transplants but he believes there are some significant advantages to their approach. I think we can guarantee a better quality of the organ and we have a long, long time to check the quality of the organ and rule out infection, he says. That is the major advantage and thats the same for other operations: a live-donor kidney transplant is better than a deceased-donor kidney transplantation for sure. But the drawback is that you expose the person to surgical risk which, of course, you dont do with the deceased donor.
Ultimately, Brnnstrm believes that it wont be long before a baby is born successfully from a deceased donor as well. I think its going to work, he says. Definitely its going to work.
The debate over whether live or dead is preferable may be a relatively brief one. Brnnstrm and his colleagues in Gothenburg are also currently working on an artificial, bioengineered uterus that would make donors no longer necessary. This process would most likely take a small number of stem cells from a womans blood or her bone marrow and these would become the basis of a 3-D scaffold into which new cells are added. It is in the early stages, but the Swedish team have already had promising results in experiments with rat uteruses.
Its enough for me to start this project and then I will let other people grow it, says Brnnstrm, who is 58. But, of course, Im optimistic otherwise I wouldnt start it. I would say 10 to 15 years.
The success of uterus transplants could provide inspiration to some other eye-catching medical advances. Now that women who were born without a womb have had children, its tempting to wonder: what about men? Neither Smith nor Brnnstrm rules out the possibility of a uterus being implanted in a man or transgender woman and them going on to become pregnant, though they stress that the surgery would be intimidatingly complex and its not something their teams have considered. Any patient would most likely need to be castrated and a neovagina created. Perhaps the biggest issue would be hormonal: androgens, male sex hormones, could endanger a pregnancy and would need to be counteracted by high doses of exogenous hormones. Even then there are concerns about whether the foetus would receive sufficient and consistent blood flow.
Such experiments have not even been trialled in animals yet, which leads most experts to predict that we are decades away from a breakthrough with humans. Its possible it could work, but youd have to fashion a new vagina and all sorts of things, says Smith. It would be technically much more difficult because you havent got the structure there to start off with.
Uterus transplants, meanwhile, are part of a growing demand for surgical procedures that improve the quality of a patients life, rather than operations to keep them alive. Last year, doctors at Stellenbosch University in South Africa performed the worlds first successful penis transplant; the recipient, a 21-year-old man from the Xhosa ethnic group whose circumcision went wrong, made his girlfriend pregnant soon after. The procedure is expected to be especially popular among the thousands of soldiers who have experienced genital damage from IEDs in Afghanistan and Iraq.
All transplants are expensive and the difficulty of finding funding for uterus surgery may mean that demand outstrips supply. Smiths team, Womb Transplant UK, is currently trying to find 500,000 to continue its work, but it has only raised 40,000 so far.
For Brnnstrm, though, the fact that the transplant does not save a life misses the point. We treat IVF, we treat causes of infertility chlamydial infections and so on and the taxpayer pays for that, he says. Why should you not treat this type of infertility where some women are unfortunate to be born without a uterus or have cervical cancer at an early age? Its actually a justice for these women that they should also get this treatment if we have it.
Lollo Wsterlund, at home in Sweden with her son Cash-Douglas, who has just turned one, certainly makes a strong emotional case. Its been life saving for me, she says. I was born without, why shouldnt I be able? If theres a chance to get a baby or be pregnant, or just to be normal, like everybody else why not? Whos the one saying: No, you dont have the right to do that? Its life saving for me, because I was so sad for so many years.
She looks at Cash-Douglas, his huge brown eyes, long eyebrows and tiny button nose, and sighs: Im just so in love with him. Hes perfect.
Making babies: fertility under the microscope
1923 The female reproductive hormone oestrogen is discovered. Followed by the discovery of progesterone, which has often been dubbed the hormone of pregnancy.
1935 The male sex hormone testosterone is discovered. Responsible for normal sperm development.
1943 Synthetic hormone supplements become available with the aim of helping those who had lower levels of the reproductive hormones needed in conception.
1944 Dr John Rock and his assistant Miriam F Menkin succeed in fertilising four ova at the Free Hospital for Women, Massachusetts. This is the first successful in vitro fertilisation of human eggs.
1953 Dr Jerome K Sherman, after establishing the worlds first human semen cryobank in Iowa City, discovers how to freeze and thaw sperm resulting in the first successful human pregnancy using frozen sperm.
1968 Sir Robert Edwards achieves fertilisation of a human egg in the laboratory.
1978 Louise Brown is born in Oldham General Hospital in England, and makes history as the first test tube baby. She is the first success story of in vitro fertilisation after 103 previous attempts by Patrick Steptoe and Robert Edwards.
1981 The birth of Elizabeth Jordan Carr, first child born via IVF in the US.
1984 Zoe Leyland is born in the US, the first successful birth from a frozen embryo. Similarly, Ricardo Asch pioneers Gamete Intrafallopian Transfer (Gift), involving the placing of eggs and sperm directly into the fallopian tubes.
1985 First successful gestational surrogacy.
1992 First successful birth from Intracytoplasmic Sperm Injection (ICSI), a procedure in which a single sperm is injected directly into the egg.
1997 Introduction of Cytoplasmic Transfer, the mixing of the genes of three people, where the extra cellular material from the donor egg is used to help fertilise the mothers egg.
1998 Scientists are able to select the sex of child by using technique that separates the X and Y chromosomes.
2009 Japanese scientists create primordial gamete cells in a petri dish, once injected into the ovaries and sperm of mice they find that the cells develop to maturity. This gives hope for the future of synthetically generated gametes (egg/sperm cells) in fertility treatment.
2014 The first live birth from a uterine transplant takes place in Sweden.
By Hannah Meneer




